
views
What is peripheral neuropathy?

Neuropathy is a condition that affects your peripheral nervous system. It’s a broad term that encompasses over 100 different kinds of nerve disorders or nerve damage caused by diabetes, injury, or other underlying conditions. Peripheral neuropathy (PN) can impact sensory, motor, or automatic nerves (or several nerves at once), meaning a patient might show a broad range of symptoms and need several types of treatment at the same time to manage their symptoms. Your peripheral nervous system is all of the nerves outside of your brain and spinal cord (central nervous system). Sensory nerves tell you how things look, feel, or smell and give you sensation in your feet. Motor nerves control how you move, walk, and balance. Automatic nerves carry signals to your glands and organs that you don’t consciously think about, like bladder control and heartbeat regulation.
Symptoms
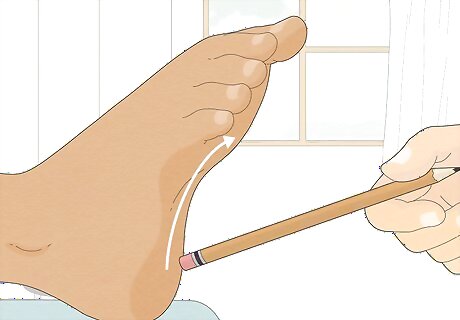
Dulled feeling, numbness, or tingling These are usually the first symptoms to appear and begin in your toes before they move to your foot and get worse or more painful. Some neuropathic patients describe feeling an “invisible sock” on their foot that muddles their feeling. If you suspect your feet are losing sensation, close your eyes and ask a friend to lightly run a pen or pencil over the tops and bottoms and see if you can feel it. Compare your foot’s ability to feel with an unaffected part of your body’s, like your thigh or arms.

Burning sensation, pain, or sensitivity to touch As the tingling feeling spreads, it becomes more uncomfortable or painful. The pain can feel like a burning or freezing sensation, or it can be sharp, jabbing, or shooting. The surface of your skin may become hypersensitive to touch, making it difficult to sleep with blankets or sheets. Neuropathic pain is often worse at night than it is during the day. The pain can be constant or periodic—it depends on which nerves are affected and the underlying cause of the neuropathy. Most of the time, the pain will happen on both sides of your body. It’s possible but rare to have neuropathy in just one foot.

Weakened foot muscles or loss of balance and coordination If your motor nerves are affected, you might experience weakness or fatigue in your foot muscles, making you more prone to clumsy trips and falls. Your balance and walking coordination may suffer, and it’s possible you won’t be able to sense where your feet are in space. Motor nerve damage may also cause muscle twitches, cramps, or spasms and difficulty walking or moving your feet.
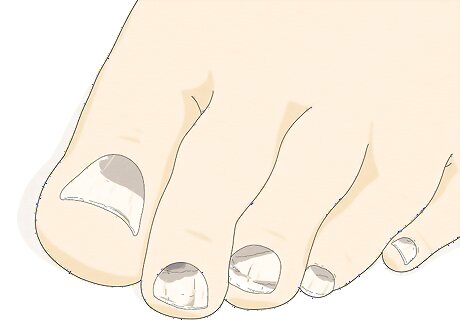
Changes in your toenails or the skin on your feet Look for thickened, brittle, or discolored toenails as well as dry or flaky skin on your toes and feet. As you lose sensation, you become less aware of injuries or traumas (like ingrown nails, stubbed toes, or ill-fitting shoes) that damage your foot health. These injuries compact over time and affect your foot’s appearance. If your neuropathy is caused by diabetes, you may also experience fungal infections under your toenails from the high levels of glucose in your blood. If automatic nerve damage keeps your feet from sweating, the skin can become dry, flaky, or cracked over time.
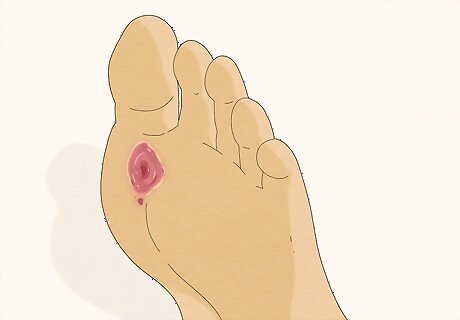
Ulcers on your feet or toes Small cuts or scrapes that you would normally treat and bandage quickly might turn into ulcers (open wounds that won’t heal) when you can’t feel them. They look like dry, cracked, or red skin at first, but grow into callused, discolored rings that might have an odor if they progress. Ulcers might appear pink, red, brown, or black (if the tissue has died). They probably won’t hurt, but may become infected and grow deeper or cover more surface area on your foot. Ulcers are most common in neuropathic patients with diabetes.

A complete lack of sensation If the neuropathy progresses far enough, you may experience a total lack of feeling in your feet or other areas associated with the damaged nerves. Your feet may feel numb all over and insensitive to cuts, injuries, or other acute conditions. Ironically, the pain receptors in your skin might start working on overdrive, making normally harmless stimuli very painful, too. A lack of feeling makes it very difficult to walk, especially barefoot. As symptoms worsen, people with neuropathy often experience worse sleep and struggle emotionally to cope with and manage their pain.
Causes and Risk Factors
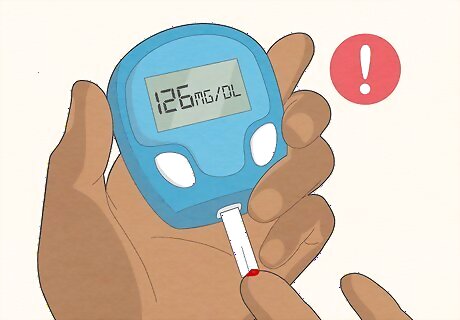
Diabetes is the most common cause of peripheral neuropathy. Diabetes elevates the levels of sugar (glucose) and fat (triglycerides) in your blood. Over time, these can damage peripheral nerves themselves, plus the small blood vessels that carry oxygen and nourishment to the nerves. Up to one half of people with diabetes will experience some type of neuropathy.
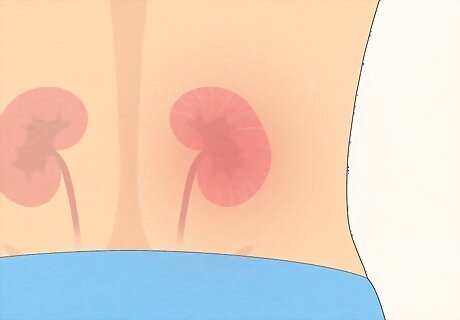
Autoimmune disorders or infections can cause neuropathy, too. Besides diabetes, there are a number of other underlying medical conditions that might trigger neuropathy in your feet. Chronic kidney disease and autoimmune issues like rheumatoid arthritis or lupus are common culprits, as well as severe infections like HIV/AIDS, shingles, or hepatitis C. Other possible causes include: Low levels of vitamins B1, B6, B12, and others Metabolic diseases Poor circulation in the legs Underactive thyroid gland Bone marrow disorders or tumors Certain genetic disorders

Physical injury is a common cause of single-nerve neuropathy. Traumas like falls, auto accidents, sports injuries, or surgical procedures can stretch or compress nerves, or detach them from the spinal cord entirely. Things like arthritis or repetitive, forceful activities (like years of pitching in baseball or working with heavy tools) can cause ligaments to swell and constrict nerve pathways, too. Sometimes, an ill-fitting cast, brace, or splint can cause neuropathy even when the original injury did not.

Neuropathy can be a side effect of medication or toxic substances. Neurological issues are complex, and it can be difficult to nail down a specific reason for neuropathy. It could be an inherited genetic disorder, or a combination of lots of different factors. There are also a number of miscellaneous causes that show up more rarely than diabetes or injury, including: Heavy alcohol use over a long period of time Poisoning from lead, mercury, glue, or toxic solvents Chemotherapy Side effects from drugs for cancer, seizures, and high blood pressure
Diagnosis
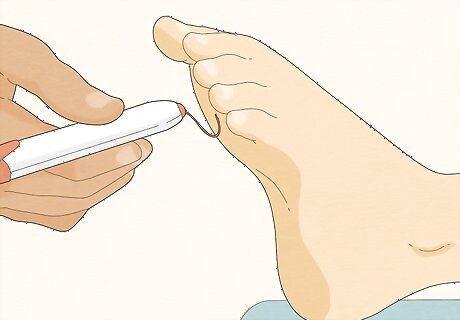
See your primary care physician as soon as you notice any symptoms. Let them know your symptoms as well as your family and medical history. The doctor will do a physical examination of your feet and order a few tests to rule out other causes of nerve damage. If you have diabetes, have your feet professionally examined by a doctor at least once a year. Some of the most common testing techniques include: Touching a tuning fork to your toes and feet to see if you can feel vibrations. Touching your toes and feet with a nylon strand to test if you can sense it (a monofilament test). Testing your balance and watching how you walk. Testing your blood for thyroid problems, kidney disease, or low vitamin B12 levels.
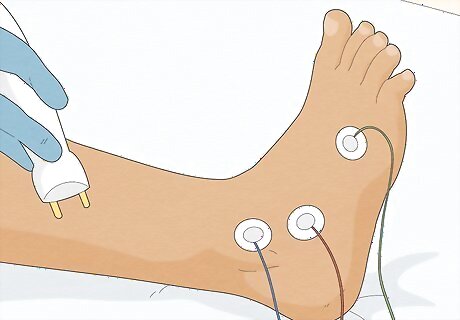
Get a referral to a neurologist to confirm you have neuropathy. If your doctor can’t diagnose you outright, you’ll probably undergo several specialized nerve tests to assess nerve damage and pinpoint the cause. The total testing time takes 20-90 minutes (depending on how many you need) and the results are available almost immediately, unlike other lab tests. The nerve tests might include: An EMG (electromyography) test to determine whether muscular weakness is due to muscle or nerve issues. AN NCV (Nerve Conduction Velocity) test to measure the speed of electrical impulses in your nerves. AN SSEP (Somatosensory Evoked Potential) test to see if the nerves connected to the spinal cord can send and receive information.
Treatment

Treat the underlying cause of neuropathy, like diabetes or infection. Discuss a treatment plan with your doctor that targets the primary cause. If you have diabetes, for example, strive to control your glucose levels with a strategic diet, exercise, and frequent testing to reduce symptoms. Create a self-care plan to prevent injuring your desensitized foot (like wearing padded slippers around the house) to encourage nerve regeneration. Use prescribed immunosuppressive drugs like prednisone or azathioprine to control inflammatory or autoimmune issues. When you correct the underlying issue, the affected nerves begin to recover and your symptoms will gradually fade. There is no direct cure for neuropathy itself. The treatment lies in the cause of the symptoms.

Take prescription medication to manage pain. There are many options when it comes to pain management. Inquire about antidepressants like nortriptyline or desipramine, which increase neurotransmitters in the spinal cord to reduce pain. Anticonvulsants that prevent seizures, like gabapentin, also help regulate your nervous system. If you’re wary of medication, try using a topical cream, patch, or spray like lidocaine. Remember that these medications treat pain, but do not correct nerve damage. Ask your doctor about potential side effects of any medication that’s considered for your treatment. OTC medications like ibuprofen or acetaminophen may not be effective for fighting nerve pain.
Get physical therapy to improve motor skills and relieve nerve pressure. Follow your physical therapist’s regimen of leg and foot strengthening exercises to regain control of your walking, coordination, and balance. Incorporate ergonomic chairs into your home and office to alleviate tension on your lower body nerves, and try out supportive, therapeutic footwear designed to assist with walking and reduce pain in your feet. Take a break from active, high-impact hobbies and sports until your symptoms are under control. Consider using a bed cradle while you sleep. It’s a device that keeps sheets and blankets off your pain-sensitive feet at night. Along with pain medication and treatment for the primary cause, physical therapy can greatly improve your quality of life and range of motion.

Undergo surgery in rare cases involving tumors or severe injury. If a tumor or traumatic wound is constricting a nerve, your doctor may recommend surgery to remove or correct the issue. In some cases, a spinal cord stimulator may be implanted to provide low-level electrical impulses to your spine for pain relief.
Prevention
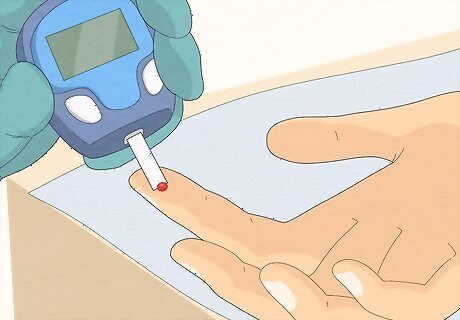
Proactively manage your diabetes. Monitor your glucose levels frequently and strive to keep them within a healthy range since high glucose is a direct contributor to neuropathic symptoms. In addition, talk to your doctor about healthy blood pressure and cholesterol goals and how to achieve them. Follow your diabetes meal plan closely. Opt for fresh produce, beans, whole grains, lean meats, fish, and low-fat milk and cheese.
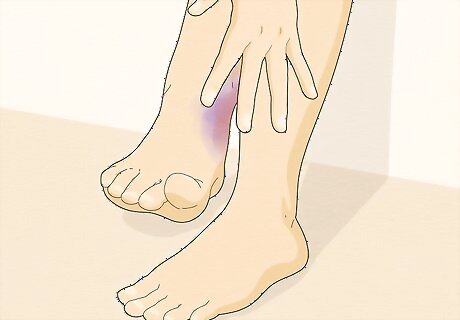
Look at and examine your feet for injuries daily. If you have diabetes, pay extra close attention to your feet if you suspect you’re losing sensation. Compare your feet’s sensitivity to other body parts and look for cuts, scrapes, or wounds that you didn’t feel. Speak to your doctor as soon as you suspect you might have any symptoms of neuropathy. Have a medical professional examine your feet at least once a year.

Get regular exercise, eat a healthy diet, and cut back on alcohol. Work out at least a few times a week to control blood sugar, strengthen your muscles, and reduce pain. Do low-impact activities that improve or prevent neuropathy symptoms like swimming or walking. Eat lots of fish, nuts, and whole grains—it’ll help you manage your weight, correct nutritional deficiencies, and improve digestive issues that might be affected by automatic neuropathy. Try to quit smoking to relieve symptoms and prevent other health issues. Limit your alcohol intake to 1 drink a day if you’re a woman or a man over 65, or 2 drinks a day if you’re a man under 65.




















Comments
0 comment