views
Common Symptoms
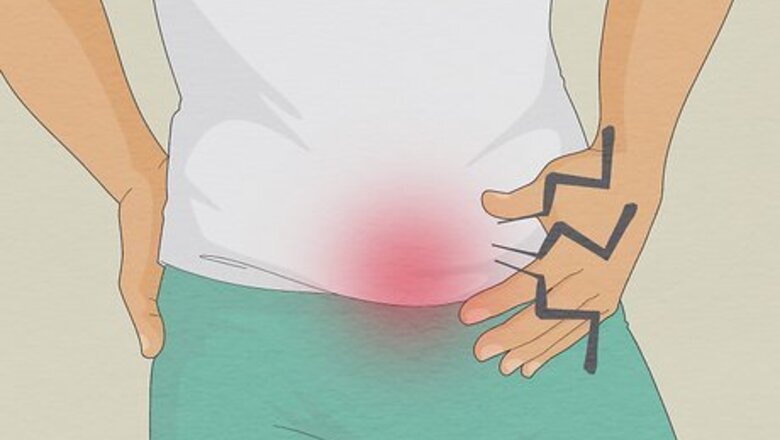
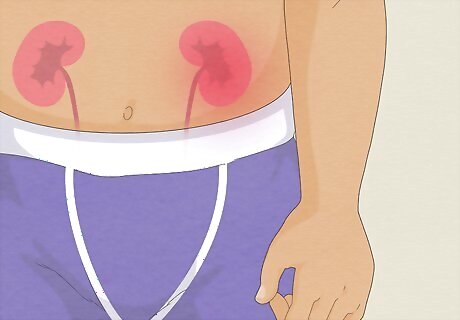
Pain or discomfort in your lower abdomen or pelvic area: Over time, the swelling spreads outwards to the testicle, vas deferens, and other areas. Depending on the severity, this might feel like pain or discomfort in your abdomen, side, or pelvis. Abdominal pain may increase gradually and coincide with testicular pain.

Testicular pain that comes on gradually, usually from one side: The first symptoms of epididymitis begin when one epididymis swells and becomes tender to the touch. This feels like testicular pain on one side that gradually gets worse over several hours. The pain may feel acute and limited to one spot on the testicle at first, but may expand over the entire testicle. See a doctor right away if you feel a sudden burst of pain in both testicles. This likely isn’t due to epididymitis and may indicate a medical emergency. The first symptoms of epididymitis usually show within 24 hours of contracting the infection.
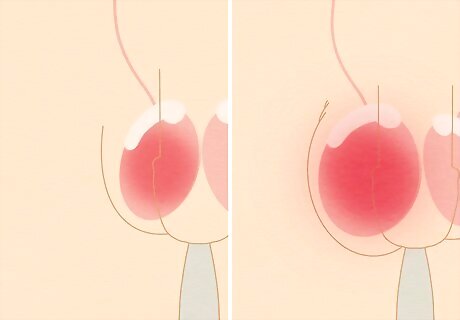
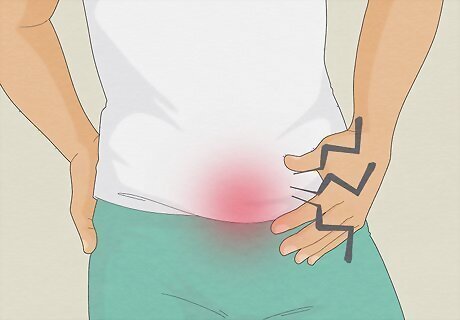
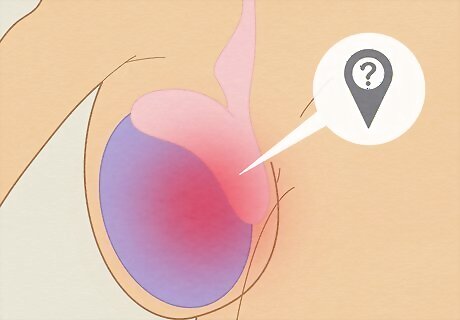
A swollen, red, or warm scrotum: A fluid bubble (hydrocele) may start to build up around the testicles, causing the scrotum to swell, look red, and feel warm to the touch. As the infection spreads, the scrotum may swell up to 4 times its usual size. The swelling is typically accompanied by pain or discomfort that might feel acute and sharp or diffuse and dull. The swelling and redness may start on one side (near the infected epididymis) and spread over the entire scrotum.

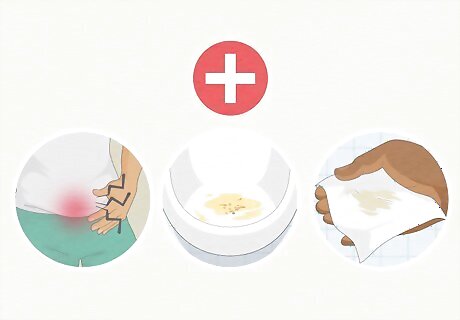
Painful or bloody urination or ejaculation: You may feel discomfort, pain, or a burning sensation in your urethra when you use the bathroom (dysuria) or ejaculate. It’s also common to feel like you have to urinate much more frequently or with more urgency, similar to a urinary tract infection. In some cases, you may also see blood in your urine or semen. Painful urination is a common symptom of a urinary tract infection (UTI). It’s possible that a UTI spread to the epididymis, causing epididymitis. If you have a UTI and not epididymitis, there won’t be any testicular or scrotal pain and swelling.
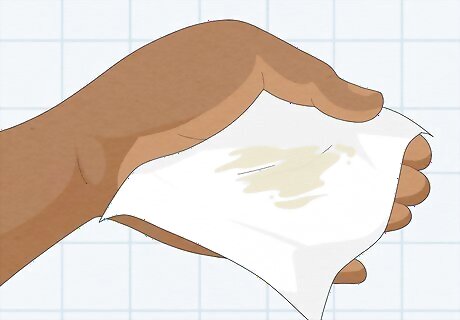
Discharge from the urethra: You may notice a clear, white, or yellowish fluid appear at the tip of the penis, indicating infection or inflammation in the urinary tract. This symptom is especially linked to epididymitis caused by an STI (sexually transmitted infection).

Fever or chills: Less commonly, you may feel a fever as your body attempts to fight off the infection. In moderate to severe cases, you may also experience body aches and chills associated with fever. A fever is any temperature above 99°F to 99.5°F (37.2°C to 37.5°C).

Symptoms lasting longer than 6 weeks: More than 6 weeks of discomfort or pain in the scrotum, testicle, or epididymis indicates chronic epididymitis. Acute (short) infections are generally treated with prescribed antibiotics, but those with chronic infections need to see a urologist for clinical management. Let your doctor know how long you’ve been experiencing symptoms. This will inform the type of treatment and care you receive for your infection.
Possible Causes

An STI from unprotected sex: Consider whether you had unsafe intercourse in the days or weeks before your symptoms began—if so, an STI is likely the cause. More than 80% of cases in men under 39 years old are caused by sexually transmitted infections, with chlamydia and gonorrhea being the most common. Chlamydia is responsible for around 60% of STI-caused epididymitis cases. Wear a condom during intercourse and talk to your partner(s) about having safer sex to minimize your risk of an STI. Epididymitis itself is not contagious, but the infections that cause it are.
Non-STI infections: In children and young men that are not sexually active, epididymitis is typically caused by an infection in the urinary tract, kidneys, or bladder that spreads to the testicles and epididymis. A history of UTIs and similar infections is a high risk factor for contracting epididymitis. Treat suspected UTIs or other infections as quickly as possible to prevent spreading into the testicles and scrotum. Reduce infection rates by practicing good hygiene and keeping the genital area clean.

Reflux of urine caused by physical activity: Sometimes, urine can backflow into the epididymis and cause an infection. This is known as chemical epididymitis and typically only happens under unique physical strain. Some of the known causes for urine reflux are: Having sex with too full of a bladder. Heavy lifting or straining. Strenuous breathing techniques like the Valsalva maneuver. Injury or trauma to the testicles or epididymis.

Recent urological procedures or catheters: Note whether you’ve had any recent medical procedures done in your groin area. In men over 35 years old, epididymitis may be the result of a procedure that introduced bacteria into the urinary tract system. These might include frequent catheters, surgery in the groin area, prostate procedures, or vasectomies. Other medical causes include urinary tract abnormalities, an enlarged prostate, and a history of frequent UTIs.

Trauma or injury to the testicles: Think back on any recent injuries to your testicles and report them to your doctor. It’s uncommon for injury to cause an infection, but it’s possible (especially if your symptoms began after trauma like a kick or a baseball to the groin).
Rare or unknown causes: In unusual cases, the root cause of epididymitis is unidentifiable. This isn’t cause for alarm since the condition is still curable when it’s acute and manageable if it’s chronic. Other times, the root cause is a rare condition or interaction with a medication, like: Viral infections such as the mumps (typically found in children). Tuberculosis, especially among men with a recent exposure or history of TB. A heart medication called amiodarone.
Getting a Diagnosis
Visit your doctor as soon as possible after you notice symptoms. Epididymitis does not clear up on its own, so it’s important to schedule an appointment with a health care provider quickly. Respond to the doctor’s questions about your symptoms, health history, and possible risk factors (like recent unprotected sex) honestly. Go to the doctor for testicular pain or swelling, pain during urination, or discharge regardless of whether you think it’s epididymitis or something else.

Undergo a physical examination from the doctor. The doctor will wear gloves and inspect your scrotum and testicles for tenderness, enlargement, and other physical indications of epididymitis. Stay calm during the exam—it may feel awkward, but it’s a necessary step towards diagnosis and treatment. If necessary, the doctor may also feel your lower back if they suspect a kidney infection or perform a rectal exam to check your prostate.
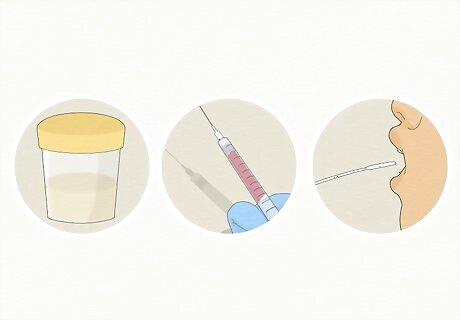
Get a full STI screening. Because STIs are the most common cause, your doctor will request tests to check for chlamydia, gonorrhea, and other epididymitis-related infections. In addition to the physical exam, you may also be asked to complete the following: A urine test. A blood test (a finger prick or blood draw). A cheek, throat, urethra, or anal swab.

Complete a urine test. Whether an STI is suspected or not, a urine test will be ordered to check for urinary tract infections or other, non-STI bacteria that may be causing epididymitis symptoms. You may also need a swab from the urethra itself to rule out urethritis (an infection of the urethra). Urine tests are the least invasive test you’ll undergo during an epididymitis diagnosis. All you have to do is pee in a laboratory cup.

Prepare to have your blood drawn. Your doctor will likely search for C-reactive proteins, erythrocyte sedimentation, or a white blood cell count (WBC) that indicates your body is fighting an infection or reacting to an abnormality. Your blood may also contain bacteria related to the infection. If you get nervous about needles, stay hydrated and eat a meal before your appointment. Focus on your breathing during the needle poke.
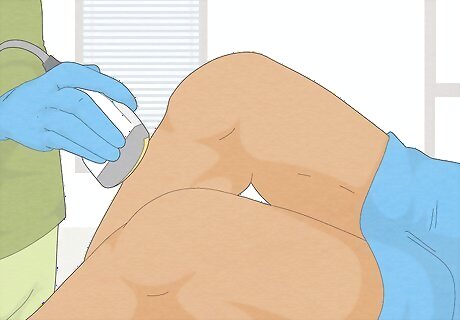
Receive a scrotal ultrasound. An ultrasound isn’t always necessary, but may be ordered to confirm you’re not experiencing testicular torsion (twisting of the spermatic cord(s)), which is a surgical emergency. It will also help pin down a diagnosis if your medical history, physical examination, and lab tests are inconclusive. Ultrasounds are painless tests that look at body tissues with sound waves. The technician will look for structural problems around the epididymis. In some cases, a CT scan or MRI may be ordered to rule out other causes of swelling and pain like cancer, gangrene, or hernia.
Treating Epididymitis
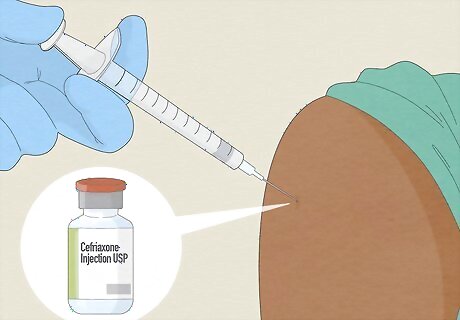
Complete a full course of prescribed antibiotics. Since the majority of cases are caused by bacteria, a 2-week dose of antibiotics is the standard treatment. The exact prescription depends on whether the cause was an STI or not. However, most sexually active men will receive presumptive therapy for STIs (a prescription to treat an STI before a positive lab result comes in) to prevent the spread of infections like chlamydia or gonorrhea. Most regimens includes a 500mg dose of Ceftriaxone (likely delivered as a shot) plus 1-2 Levofloxacin or Doxycycline pills per day for 10+ days. If an STI is the root cause, your partner(s) will be prescribed antibiotics as well. The infection will be cured by the end of your antibiotic prescription (typically 10-14 days), but some discomfort may take several weeks to go away.

Treat pain with non-steroidal anti-inflammatory medication (NSAIDs). Your doctor may prescribe or recommend anti-inflammatory pain medicine, like Ibuprofen, to reduce testicular pain or swelling while the antibiotic clears up the infection. If pain and swelling continue after 10 days of taking NSAIDs, follow up with your doctor. In general, adults and teens can take 400mg of Ibuprofen every 4 hours or as needed.
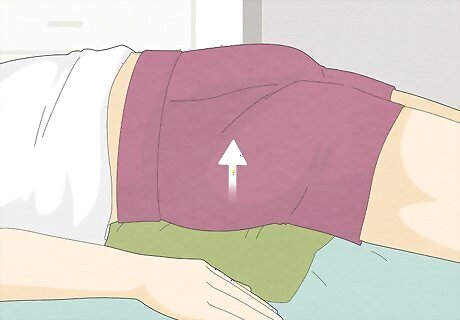
Rest and keep your scrotum elevated. Commit to several days of bed rest to reduce stress on your groin and alleviate pain and discomfort. Try laying down on your back with a pillow, towel, or rolled shirt underneath your scrotum to keep it elevated and reduce swelling. When you're not laying down, wear supportive underwear that keeps your scrotum relatively still and cradled.

Apply a cold compress to reduce swelling. Ice reduces blood flow, which alleviates inflammation and acute pain. Wrap an ice pack in a cloth and apply it to your scrotum for no more than 20 minutes at a time to prevent skin damage. Don’t apply cold compresses or ice packs directly to the skin, especially in a highly sensitive place like the scrotum or groin.
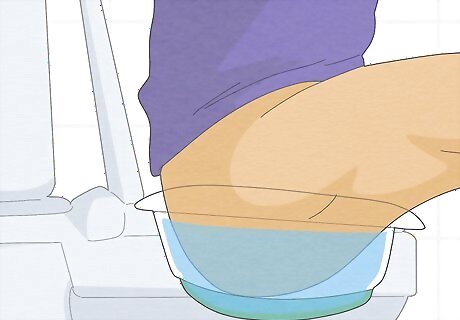
Take frequent warm or sitz baths for chronic epididymitis. Soak your abdomen, groin, and scrotum in warm water for about 30 minutes at a time to manage pain. Fill up your bathtub with 3-4 inches (7.6-10.1 cm) of warm water, or place a sitz bath bowl on top of your toilet and fill it with warm water before taking a seat. Take a sitz bath as often as you need. Your doctor may recommend adding salt or medicine to the water if baths are part of your long-term treatment plan.

Follow up with your doctor if you don’t feel improvements in 3 days. Notice whether your symptoms begin disappearing after you start your antibiotics. If there’s no relief within 72 hours, call or visit your doctor for a reevaluation—it’s possible there’s a stronger infection or another cause of symptoms that needs to be treated. Some symptoms, like scrotal swelling, may linger after you finish your antibiotics. Check with a doctor to confirm if you need additional treatment. In very rare and severe cases, surgery may be required to remove abscesses or malformed portions of the epididymis.


















Comments
0 comment