
views
There were times, not far back, when the birth of children via C-section used to be an anomaly.
Women belonging to my mother or grandmother’s age would instinctively presume that there were acute complications if the baby is born via C-section. Today, I have lost the count of the number of babies born to my near and dear ones via this surgery.
If you look around, you will learn the same. Numbers also suggest the same trend.
The latest government data shows that Indian women are opting for C-sections to deliver children more than ever.
While the birth of babies via C-section (Caesarean section) deliveries has been on the rise for over a decade now, no sense of urgency has been shown by the government to curb the trend.
Data auditing, adoption of Robson’s classification and undertaking sensitisation drives among women could have been the immediate steps.
The latest National Family Health Survey (NFHS) data shows the rate of C-section deliveries increased from 17% in 2015-16 to 22% in 2019-21. In 2005-06, the rate stood at 8% of the total deliveries.
Due to the unregulated market and no clear protocols, India is now facing an epidemic of C-sections which is counted among the “major” surgeries.
From 4 lakh C-section deliveries in public health facilities in 2008-09, the number escalated to 19 lakh deliveries in 2019-20, a jump of almost 320%.
The numbers show that such deliveries are particularly high in private sector health facilities. However, it doesn’t mean that they are not increasing in government hospitals.
‘EPIDEMIC’ OF C-SECTIONS
The available data at Health Management Information System (HMIS) in private hospitals shows C-sections have quadrupled from 4.60 lakh in 2008-09 to 20.5 lakh in 2018-19.
Between 2019 and 2020, around 1.37 crore deliveries took place in public hospitals, of which 19.35 lakh or a little over 14% were through C-section surgery.
Similarly, in private hospitals, of the almost 65 lakh deliveries, around 22 lakh or 34% of the deliveries were via C-section.
WHY IS IT A CONCERN?
Access to C-section can reduce maternal and neonatal mortality.
The World Health Organization (WHO) does not recommend a target rate for countries to achieve, but says that every effort should be made to provide such procedures to women in need.
The international healthcare community, including the WHO, has considered the ideal rate for C-sections to be from 10% to 15% (of the total deliveries).
Not only overall, the rate helps in monitoring the use of C-section across districts and state-wise.
To put it in perspective, C-section deliveries should not be the first option because :
A. It’s not the natural way to deliver a child.
B. Because it’s not the natural way, the effects of C-section rates on other outcomes, such as health of the mother, health of the child, psychological or social well-being, are still unclear. WHO says more research is needed to understand the health effects of C-section on immediate and future outcomes.
A study conducted by IIM, Ahmedabad labels the intervention as “medically unjustified”. “For the newborn, it means delayed breastfeeding, lower birth weight, respiratory morbidities, increased rate of hospitalisation, lower Apgar scores and its implications in the long run.”
WHY C-SECTION?
The NFHS data shows that Caesarean deliveries are more common among first births and its rate is higher in urban areas than the rural areas.
More educated women are likely to undergo this method due to various reasons such as late marriages and delayed family planning leading to complicated pregnancies.
Government data shows mothers in households in the highest wealth quintile are much more likely to deliver through C-section (39%) than mothers in households in the lowest wealth quintile (7%).
Reason: Wealthy families prefer visiting private hospitals and the chances of delivering a child via C-section are high there, data proves.
“C-section is a supplier-induced demand driven by monetary incentives,” health economist Indranil Mukhopadhyay had told me in 2019, when I was working on the same subject for a different publication.
Here, the supplier is a hospital who can sell the product (in this case, C-section) to a patient who has limited information.
MIDWIVES ARE THE FIRST ANSWER
To control the ‘shift away’ from natural delivery procedure, it is crucial to formulate a balanced mandate which does not deny access to the procedure, but lays conditions on the use of surgery.
The first step that India needs to take is to strengthen the workforce of midwives and build a culture of midwifery.
Many in India may end up relating midwives to the ‘dais’ of old times and assume midwife as an old-aged, untrained and unhygienic lady with a set of outdated opinions.
However, midwives are not even close to this. In fact, there are a few evidences that trained midwives are as good as doctors in handling uncomplicated births.
The data by WHO shows that 83% of all maternal deaths and newborn deaths globally could be averted with midwifery care. It found that pregnant women, who are assisted by midwives, were less likely to give birth prematurely or lose their babies.
In several developed countries, such as in Finland or the UK, midwives are recognised as part of healthcare workers and take care of pregnant women.
India needs to unfollow the American model where obstetrics dominate the pregnancy and childbirth care. Instead, look at some of the European nations where more than 75% of childbirth are handled by midwives.
This category of healthcare workers is known as trusted companions of women throughout their pregnancy, birth and the period following childbirth.
“A system of triage to identify normal and complicated cases will help reduce the C-section based deliveries,” Dr Rinku Sensupta, a senior gynaecologist, who specialises in natural birth, agreed.
“Midwives supported by a team of specialists would help in reducing the need to hasten labor that results in childbirth by Caesarean section,” she said.
While India has started working on the creation of the cadre, remarkable progress is yet to be seen as it was slightly derailed due to Covid-19. In 2020, the first batch of professional midwives in India had initiated their training.
The new guidelines on midwifery in India were released in December 2018. A cadre of Nurse Practitioner in Midwifery (NPM) was announced to be created in accordance with International Confederation of Midwives standards. It said that NPM will be a registered nurse-midwife with an additional 18 months of post-basic training in midwifery.
As per the WHO, India has over 20 lakh nurse-midwives and nearly 9 lakh Auxiliary Nurse Midwives (ANMs) and the Government of India has committed to an additional 85,000 midwives by 2023.
HOW CAN THEY HELP?
Not only monetary incentives, shortage of resources in private nursing homes also push gynaecologists or doctors to conduct C-sections as they do not have the resources to handle women in labour pain for an undefined period. The process of labour can stretch for as long as 48 hours. If a hospital does not have resources and staff to handle such mothers in pain, they will opt for C-sections.
In private hospitals too, the solo practitioners become the face for their patients.
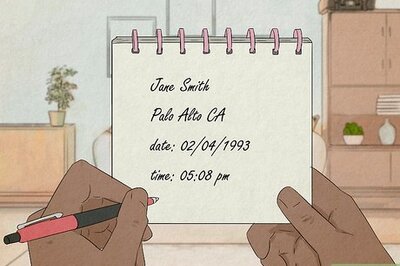
Anita (for instance) and her family will look for her doctor X throughout. She will expect doctor X to be around until she delivers the child.
If in a month, 25 deliveries are lined up, it is impossible for the doctor X to remain available for all of them. Hence, they need to plan the deliveries in advance which can be done using C-sections — unethical, but a reality.
Here, if uncomplicated pregnancies were being handled by midwives, the doctors can be relieved to focus only on complicated cases out of those 25 due deliveries.
It is not a magic wand. The introduction of midwives will not solve the problem immediately as families may still look for doctors, disregarding them as mere nurses.
The road ahead is long and needs a culture and mindset shift.
Read all the Latest India News here


















Comments
0 comment