
views
X
Trustworthy Source
Mayo Clinic
Educational website from one of the world's leading hospitals
Go to source
It is a good idea to see your doctor to find out what is causing your nasal congestion, but if your symptoms are not too severe, then you can decongest your nose using some simple strategies.
Thinning Out Nasal Mucus

Apply a warm washcloth to your nose and face several times a day. The heat will open up your blood vessels and make it easier for fluid to escape. Place a washcloth in warm water but make sure that the water is not too hot so that you do not burn your skin. Ring out the excess water and then place the washcloth over your face and nose. Relax for about five to 10 minutes, and then remove the washcloth.

Inhale steam from a warm bath or shower. Inhaling steam from a shower or bath can help to thin out nasal mucus as well. Take a warm shower or bath and inhale the warm steamy air. You can also sit in the bathroom with hot water running in the tub or shower for about 10 – 15 minutes. The steam will fill the room and help to loosen up mucus in your nasal passages.

Use a humidifier or vaporizer. Dry air in your bedroom and the rest of your house can aggravate a congested nose. A humidifier or vaporizer can help by releasing water vapor into the air, which helps to reduce dryness. Try using a humidifier at night to increase moisture levels in the air and help to thin out your mucus.

Stay hydrated. Drinking plenty of water will thin out your mucus and may help prevent your sinuses from getting blocked up. Aim to drink eight glasses of water per day to ensure proper hydration. Sip water throughout the day, and enjoy other hydrating beverages such as juice, decaffeinated coffee, and caffeine-free herbal teas.
Clearing Mucus From Your Nose

Blow your nose gently. Blowing your nose hard and fast can get rid of germs and mucus from your nostrils, but the high pressure can also force it back into your nose and sinuses. Instead, blow your nose gently to get more mucus out of your nose. Using a soft tissue, close one nostril by pressing your finger against one side of your nose, and blow gently out the open nostril.

Sit up. Although you may want to lay down to rest while you are sick, laying down can make it harder for your sinuses to drain. Sitting up rather than laying down will help to drain your nose. Sitting up will pull the fluid out of your nose and make it easier to clear. Try using pillows to prop your head up at night and also when you are resting.

Wash out the mucus with a neti pot. Pouring lukewarm water inside your nose can help clear the mucus buildup. Try using a neti pot, which is a container used to pour salt water through a long thin spout into the nose. Fill the neti pot with a solution of lukewarm water and salt. This solution is meant to mimic natural body tissues and fluids. Mix about 16 ounces (1 pint) of lukewarm water with 1 teaspoon of salt to create the solution for your neti pot. To use a neti pot, tilt your head sideways over the sink and place the spout of the neti pot in the upper nostril. Breath through your mouth and gently pour the solution into your upper nostril so that the liquid drains through the lower nostril. Repeat on the other side. Rinse the device after each use with sterile, boiled or filtered water.
Using Decongestant Medicines

Be aware that decongestant medicines and sprays can have some serious side effects. If you are on any medications or if you have a medical condition, then you should speak to your doctor before trying any over the counter medicines or nasal sprays. For example, if you have an enlarged prostate, glaucoma, heart disease, high blood pressure, or thyroid disease, check with your doctor or pharmacist before use because all decongestants, including sprays, can worsen these conditions. Your doctor can advise you on what medicines are and are not appropriate for you. Keep in mind that the potential side effects of decongestants include: Irritation to the lining of your nose, which may include nosebleeds A skin rash Headaches Dry mouth Restlessness or anxiety Tremor (uncontrollable shaking and trembling) Problems sleeping (insomnia) Rapid and/or irregular heartbeat Noticing your heart beating inside your chest (palpitations) Increased blood pressure

Consider taking an over-the-counter decongestant. Over-the-counter decongestants (those not requiring a prescription) include phenylephrine and pseudoephedrine as main ingredients. They work by constricting the blood vessels in the nose. This reduces how much blood flows through the area so that swollen tissue inside the nose shrinks and air can pass through more easily. Phenylephrine comes as a tablet, a liquid (spray), or a dissolving strip to take by mouth. Also, it is an ingredient in many cold/flu medications. Follow directions on the bottle on its use. Pseudoephedrine comes as a regular tablet, a 12-hour extended-release (long-acting) tablet, a 24-hour extended-release tablet, and a solution (liquid) to be taken by mouth. Follow the directions on the package.

Try a decongestant nasal spray. Nasal sprays help to clear congestion by shrinking blood vessels in your nose and reducing swelling. Ask your doctor about a prescription nasal spray or buy an over-the-counter nasal spray. To use a nasal spray canister: Gently blow your nose to clear it of mucus before using the medication. Shake the canister before using it. Keep your head upright and breathe out slowly. (Tilting back your head can lead to increased absorption into your body and increase side effects.) Use your finger on the free hand to close the nostril on the side not receiving the medication. Place the tip of the canister in your nostril and press down as you begin to breathe in slowly through your nose. Repeat these steps for the other nostril. Try not to sneeze or blow your nose just after using the spray.

Limit the length of time that you use a nasal spray. Do not use a nasal spray for more than three days. Using a nasal spray for more than three days can lead to rebound congestion, a condition in which the congestion returns. If your congestion lasts more than three days, use a nasal spray for the first three days then switch to an oral decongestant. Do not use both at the same time as this can increase risk of side effects.
Getting Medical Help
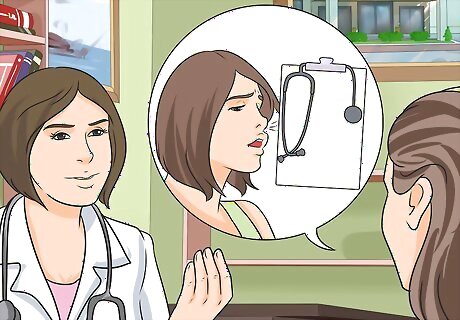
Tell your doctor about all of your symptoms. Your doctor will take a detailed history of your current symptoms and past medical history as well as any associated symptoms/signs such as fever, headache, coughing, shortness of breath, etc. During your exam, your doctor will look at the inside of your nose with a penlight, check your ears for any fluid buildup, touch your cheekbones and/or forehead for sinus tenderness, and feel for any swollen lymph nodes around your neck. Your doctor may also order blood work to check the number of immune fighting cells present in your body (WBC). If they are elevated, chances are there is an infection or something causing inflammation such as allergies. Your doctor may refer you to an ENT physician (ear, nose, and throat doctor) for the referral if further expertise or tests are needed.
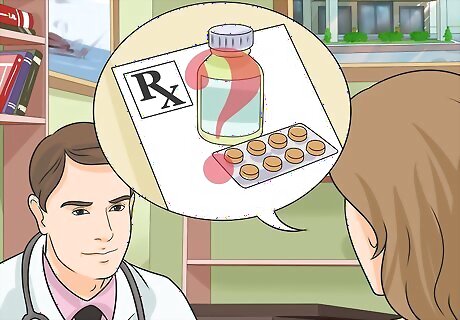
Ask your doctor about prescription medications. Most nasal decongestants can be purchased over the counter without a prescription. Depending on the cause of the congestion, other medications may be needed. For example, sinus infections may require antibiotics to fight bacteria, while asthma and other serious inflammation disorders may require the use of steroids.

Call your doctor if you experience any severe symptoms. In some cases, congestion may become severe or be accompanied by other serious symptoms. Call your doctor right away if you experience any of the following: Nasal congestion is lasting more than ten days. You have a high fever, and/or it lasts more than three days. Your nasal discharge is green and is accompanied by sinus pain (pain around your cheekbones or forehead) or fever. This may be a sign of a bacterial infection. You have asthma, emphysema, or you are taking medications that suppress your immune system, such as steroids. This may increase the risks of infections. You have blood in your nasal discharge or a persistent clear discharge after a head injury. The clear fluid or blood may be coming from your brain after a head injury.


















Comments
0 comment